
Dental issues can not only affect your oral health but also have a negative impact on your overall health and life. Even simple tasks such as chewing can become difficult and routine activities can become challenging with symptoms such as headaches due to dental problems. One such dental issue is pericoronitis. It is an infection affecting the soft tissues which surround the crown portion of a partially erupted tooth.
This article helps you understand every aspect related to pericoronitis. What exactly is this oral issue, what are its causes, symptoms, associated risks, treatment options, and recovery time?
What is Pericoronitis?
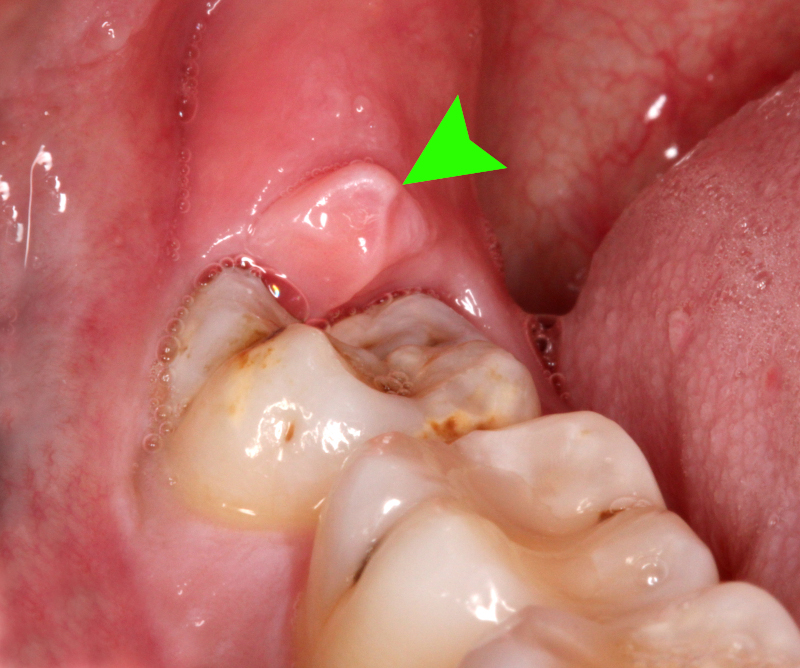
When there is inflammation in the gum tissue surrounding the crown portion of a tooth, it is known as pericoronitis. In this condition, the gum tissue overlaps the chewing surface of the tooth. It usually affects the lower third molar or wisdom teeth. It is commonly seen in young adults who are in their mid-20s and who are experiencing poorly erupting wisdom teeth.

When the inflammation is mild but persistent, it is known as chronic pericoronitis. When fever, swelling, or pain occurs, it indicates the spreading of infection and is known as acute pericoronitis.
Unlike periodontal disease or periodontitis, pericoronitis occurs specifically around an incompletely erupted tooth.
What are the Causes?
Accumulation of bacteria is the number one cause for pericoronitis. When the tooth is partially exposed and has excessive gum tissue (operculum) overlapping it, bacteria and food debris can easily get trapped in between. This promotes inflammation and creates a breeding ground for infection. A pericoronal infection can develop by an abscess formation under the operculum. If left untreated, this infection can spread to the surrounding teeth, gums and other soft tissues.
The following factors can also trigger pericoronitis infection:
- Improperly erupted wisdom teeth
- Poor oral hygiene
- Excessive gum tissue
- Emotional stress and fatigue
- Pregnancy
What are the Symptoms?
The symptoms of pericoronitis may vary depending on whether the nature of the infection is chronic or acute. Listed below are the symptoms of this infection:
- Acute pericoronitis – Locked jaw or trismus, swollen gum tissue, pus discharge, difficulty in swallowing or dysphagia, severe pain near back teeth
- Chronic pericoronitis – Mild or dull ache lasting for a day or two, bad taste in the mouth, bad breath
Other symptoms include tenderness and redness in the gum tissue, swollen submandibular lymph nodes, fever, loss of appetite, and feeling unwell.
How is it Diagnosed?
Your dentist or oral surgeon will take dental X-rays to assess the area and also to rule out other causes such as dental decay. These X-rays and the symptoms can help the dentist diagnose whether it is pericoronitis or not.
What are the Treatment Options?
Generally, there are three treatment options. These are based on the severity of the infection. Most of the time, only treating the actual symptoms is the best possible approach. The treatments are as described below:
- Pain Management
This is mostly achieved with over-the-counter pain medications such as Ibuprofen (Advil), Acetaminophen or Tylenol. If the infection is limited to the tooth, the dentist cleans out the area thoroughly by administering local anesthesia. He or she may also prescribe an oral rinse to keep the infected area clean. In case of swelling or fever, the dentist may also give oral antibiotics such as Erythromycin or Amoxicillin.
- Minor Oral Surgery
If the infected molar can be used for chewing and the patient wants to retain it, minor oral surgery can be performed to remove the overlapping gum tissue flap or operculum. This allows the dentist to clean the infected area thoroughly and also prevents further accumulation of any food debris or growth of bacteria. However, sometimes, the flap of gum tissue may regrow and result in the same problem again.
- Wisdom Tooth Extraction
The third molars or wisdom teeth often erupt incompletely or in a misaligned position. In such cases, wisdom tooth extraction is often prescribed by the dentist. This treatment eliminates the risk of infection in wisdom teeth.
Sometimes, mild pericoronitis can be treated at home with thorough yet gentle brushing of the infected area with a small-headed toothbrush to help remove any trapped food debris or plaque. Oral water irrigators can also be used to flush out the debris trapped under the operculum. The area can be soothed by rinsing with warm saltwater. However, you should consult your dentist at the onset of the infection to prevent further complications rather than treating the infected area at home.
Any dentist who holds a license can treat pericoronitis. In case a surgery is required or the infection is severe, dental specialists such as an oral surgeon or a periodontist (gum surgeon) can perform suitable treatments.
What are the Associated Potential Complications?
There can be some complications such as pain and swelling around the third molars in case of pericoronitis infection. Other issues include difficulty in biting down, locking of the jaw, and in certain cases, the infection may spread from the affected tooth to the surrounding teeth and gums. In extremely rare cases, a person with pericoronitis may develop a life-threatening medical issue known as Ludwig’s angina. In this condition, the infection from the affected molar spreads to the head and neck. Another condition in which this infection spreads to the bloodstream is known as sepsis and it is also a rare life-threatening medical issue.
What is the Recovery Time?
Mostly, once the wisdom tooth or teeth has been removed, pericoronitis rarely recurs. Recovery time is around two weeks post-extraction and one or two days for symptom-specific treatment in case of acute pericoronitis.
A good oral hygiene routine, proper precautions, and regular dental visits when the third molars are erupting can reduce the risk of this dental condition. Since your dentist can periodically monitor the eruption process, he or she can take proactive action to extract the wisdom tooth or teeth early if required. The dentist can also prescribe regular professional cleaning sessions to prevent infection and inflammation. If you are experiencing any of the symptoms of pericoronitis, consult your dentist to prevent further oral complications.
References
Hazza’a A. M., et al. “Angulation of mandibular third molars as a predictive factor for pericoronitis.” The Journal of Contemporary Dental Practice 10.3 (2009): 51-58.
Nguyen, D., et al. “Common Dental Infections in the Primary Care Setting.” American Family Physician 77.6 (2008): 797-802.
Sixou JL, et al. (2003). Microbiology of mandibular third molar pericoronitis: Incidence of beta-lactamase-producing bacteria. DOI:10.1067/moe.2003.238
Blakey GH, et al. (1996). Clinical/biological outcomes of treatment for pericoronitis.
ncbi.nlm.nih.gov/pubmed/8859232
Pericoronitis: Treatment and a clinical dilemma. (2009).
exodontia.info/files/J_Irish_Dent_Assoc_2009._Pericoronits_-_Treatment_A_Clinical_Dilemma.pdf

I experience the pain of this. My wisdom tooth erupted in my third molar, and it’s getting worse every day. I experience this in the first month of February this year, but due to lockdowns, I was not able to visit my doctor. But last month, I’m so glad that my doctor texted me and do the surgery. I live with this for 7months and I’m very happy now because I get rid of it.
I’m so glad you were able to get that taken care of!
I had the same issue many years ago and it was also due to impacted wisdom teeth; so, I know how painful it can be.
Thank you, for sharing your experience! 🙂